How Can People Protect Themselves From Exposure to Known Risks Factor's of Cancer?
T he gamble of exposure to ionizing radiation is a permanent topic on the agenda of global organizations such every bit the International Commission on Radiological Protection (world wide web.icrp.org), the United Nations Scientific Committee on the Effects of Atomic Radiation (www.unscear.org), the International Atomic Energy Agency (www.iaea.org), and the World Wellness Organization (world wide web.who.int). The role of these global organizations is crucial, every bit they continuously evaluate and analyze the scientific literature on the effects of ionizing radiation and too publish recommendations and guidelines on how to safely use ionizing radiation.
There is an ongoing controversy among the scientific community about the acceptance of the linear no-threshold (LNT) model, which assumes that the long-term, biological damage caused by ionizing radiation (substantially the cancer adventure) is straight proportional to the dose, and any increase of exposure above natural background levels volition produce a linear increment of risk. The LNT model hypothesis has competing theories: (1) the threshold model, which maintains that very modest exposures to ionizing radiations are harmless; and (two) the radiation hormesis model, which assumes that radiation at very pocket-size doses can be beneficial.1
The French Academies consider that the LNT model for assessing carcinogenic risks induced past low doses, such as those delivered past diagnostic radiology, is non based on valid scientific data and might create anxiety among patients; however, they acknowledge that the model tin can be practical for the arrangement of radiation protection.2 Conversely, the International Committee on Radiological Protection and the National Academy of Sciences (Biological Effects of lonizing Radiation [BEIR] Seven report) back up the apply of the LNT model.3 The BEIR VII committee concludes that current scientific prove is consequent with the hypothesis that in that location is a linear dose-response relationship betwixt exposure to ionizing radiation and the development of radiations-induced solid cancers in humans.4
Radiations is ane of the virtually extensively researched carcinogens, merely the furnishings of low doses are however somewhat unclear. The weight of show from experimental and epidemiologic data does not propose a threshold dose below which radiation exposure does not cause cancer. If there is no such threshold, then diagnostic ten-rays are probable to induce some cancers.5
Despite the controversies found in the literature, the LNT model hypothesis remains a wise basis for radiation protection at low doses and low dose rates6 and currently represents the best means for radiation protection standards.7
OPTIMIZING RADIATION PROTECTION
Even knowing that there are several controversies regarding the quantification of risks and a lack of agreement on how to nowadays them, the best approach for radiographers using ionizing radiations in clinical exercise is to perform a medical imaging procedure post-obit the ALARA principle, which asserts that radiations doses should be kept every bit low equally reasonably doable, taking into account social and economical factors.8,ix
The ALARA principle is an accepted keystone of radiation protection optimization or in replacement thereof. Yet, it should be noted that the ALARA principle is only part of the concept of optimization. The entire concept implies, more precisely, keeping patient exposure to the minimum necessary to reach the required medical objective (diagnostic or therapeutic). In diagnostic imaging and 10-ray–guided interventions, it means that the number and quality of images are sufficient to obtain the information needed for diagnosis or intervention. In radiations therapy, ALARA only applies to normal tissue, as the dose to the target is not expected to exist as low as reasonably achievable, only rather the opposite. Use of the abbreviation "ALARA" alone and out of this context may be misleading and raise unnecessary controversy.10
The largest prospective written report published to date, which followed a large cohort of radiographers (xc,957), observed elevated risks of brain cancer, breast cancer, and melanoma amid radiographers who performed fluoroscopically guided interventional procedures (FGIPs) when compared with those not involved in those procedures. Authors also pointed out that although exposure to low-dose radiation is 1 possible explanation for these increased risks, results may also exist due to gamble or unmeasured confounding by nonradiation risk factors.11 I possible explanation for the study findings is that radiographers involved in FGIPs may not accept optimized their radiation protection. First, they may have spent more than time than needed in the FGIP room (cath lab). Second, they may take failed to take the necessary measures to be every bit far as possible from the patient (the main source of scatter radiations) and the x-ray tube when in the cath lab. Lastly, they may not have used tailored personal protective devices (eg, pb aprons, thyroid collars, protective glasses) during FGIPs.12
Radiographers involved in FGIPs tin be at risk of exceeding annual radiation dose limits and thus be at risk for long-term adverse health effects if they do not practice proper radiation protection measures and adherence to safety practices.13
The simply fashion to promote a professional condom culture among radiographers and reduce the risk to both professionals and patients is to comprise a structured radiation protection curriculum into education and training programs with a articulate set of knowledge, skills, and competences as expressed in the MEDRAPET (Medical Radiation Protection Teaching and Training) guidelines.xiv
ATTITUDES AND BEHAVIORS TO DECREASE EXPOSURE TO IONIZING Radiation IN FGIPsouthward
Education and training in radiation protection is an essential component when implementing a culture of safe among health professionals in full general.15 Even so, it is important to be enlightened that noesis of radiation protection alone is not enough, and further skills and competencies are needed to ensure education and preparation are effective. It is also essential to pay special attention to applied aspects regarding communication, teamwork, and the full use of radiation-reduction features bachelor in angiography equipment.
Good advice between the wellness intendance professionals involved in FGIPs is an important tool to improve clinical practice. Through preprocedural advice and postprocedural analysis, information technology is possible to identify pitfalls and lack of data about the FGIP and radiation protection issues. Radiographers can and should contribute to the coordination of radiations protection practice amid other health professionals working in FGIPs, ensuring that all colleagues empathise that radiations protection is the responsibleness of each individual and act accordingly. Conspicuously, irresponsible and/or ignorant beliefs from any member of a FGIP team tin be associated with significant collateral damage to the patient and personnel.
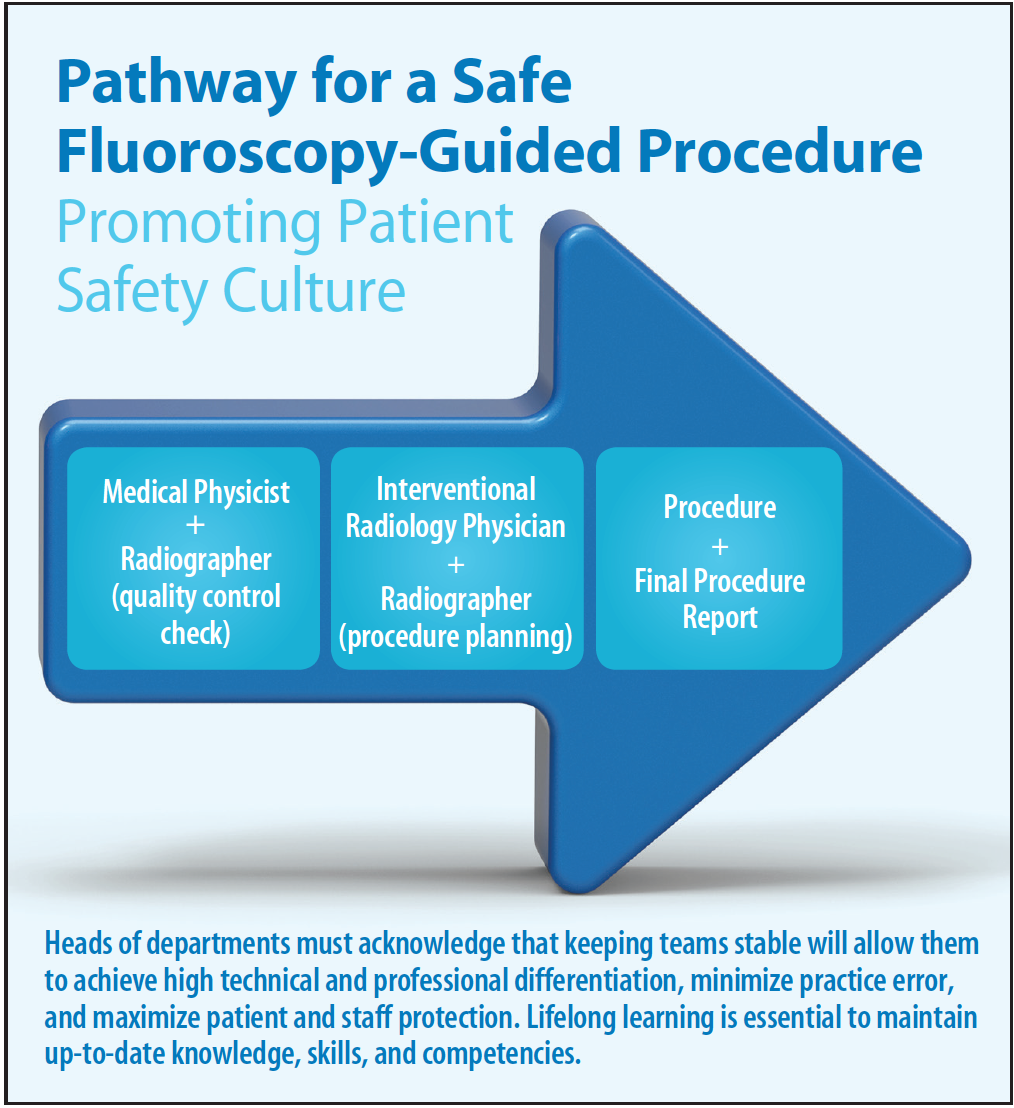
Figure 1. Pathway for a condom fluoroscopy-guided process that promotes a culture of patient safety.
Figure 1 outlines a pathway for implementing a culture of patient safety for the FGIP before, during, and later a procedure. Such a pathway volition minimize practise errors and maximize patient and staff protection.
Before the procedure begins, information technology is of import that the radiographer and the interventionist correctly place the FGIP past selecting the proper process name and imaging protocol for the clinical task to be performed. The imaging protocol should exist discussed and agreed upon with the interventionist, since the type of fluoroscopy used will affect the patient and staff dose (eg, depression, standard, or high fluoroscopy mode). A recent development in FGIP is the use of cone-beam CT for imaging and guidance. This new engineering requires well-trained and highly skilled staff, and radiographers take the main responsibleness of optimizing its use by choosing the most acceptable exposure factors to provide the required image quality, while taking into account the clinical chore and the lowest required dose.
The radiographer, together with the medical physicist, should develop dose reduction measures for FGIPs and implement them in daily practice. Dose reduction strategies will benefit patients and staff and include the option of the best exposure factors, taking into consideration the patient's anthropomorphic characteristics (exposed area, age, and trunk mass index), the clinical task, and equipment typology.
Radiation Protection Apparel and Shielding
The radiographer should pay special attention and ensure that all wellness professionals involved in FGIPs apply protective shielding devices (eg, aprons, thyroid shields, leaded goggles), protective screens (of import to reduce dose to the eye lens), and other shielding devices. Radiographers play a key part in the option, accommodation, and maintenance of the protective apparel. Procedures and frequency of routine quality assurance should be established to test aprons and their credence limits for 10-ray transmission at specific kVp values. The objective is to identify and remove equipment begetting large holes or tears that could compromise the safety of individuals using this shielding device.16,17
The radiographer should also pay special attention to the employ of personal dosimeters and positioning of the health professionals inside the room during the FGIP, as well as recommend proper placement of dosimetry badges where lower dose levels are expected in cases when being inside the room is mandatory.
SUMMARY
The radiographer has several important roles that contribute to decreasing patient and staff exposure to ionizing radiation: (1) working with the medical physicist and interventionist to implement a quality command model and develop optimized protocols; (ii) accurately identifying the type of process and imaging protocol for an individual patient; and (3) maintaining a skillful safety culture to protect patients and staff in the daily routine.
The adventure from exposure to ionizing radiation exists and is an of import focus of international organizations. Nevertheless, the harmful effects of ionizing radiation tin be macerated if the occupational exposure is maintained under recommended annual limits, the FGIP is optimized with the use of radiation reduction features on angiography equipment, and health care professionals accordingly utilize protective devices and attire.
1. Wall BF, Kendall GM, Edwards AA, et al. What are the risks from medical 10-rays and other low dose radiation? Br J Radiol. 2006;79:285-294.
2. Tubiana One thousand. Dose-effect human relationship and estimation of the carcinogenic furnishings of low doses of ionizing radiation: the joint report of the Académie des Sciences (Paris) and of the Académie Nationale de Médecine. Int J Radiat Oncol Biol Phys. 2005;63:317-319.
three. Tubiana Thou, Feinendegen LE, Yang C, Kaminski JM. The linear no-threshold relationship is inconsistent with radiation biologic and experimental data. Radiology. 2009;251:thirteen–22.
4. Committee to Assess Health Risks from Exposure to Depression Levels of Ionizing Radiation. Wellness Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII Stage 2. Washington, DC: National Academies Press; 2006.
5. Berrington de González A, Darby S. Risk of cancer from diagnostic x-rays: estimates for the Great britain and 14 other countries. Lancet. 2004;363:345-351.
vi. Valentin J. Low-dose extrapolation of radiation-related cancer risk. Ann ICRP. 2005;35:1-140.
seven. Breckow J. Linear-no-threshold is a radiation-protection standard rather than a mechanistic effect model. Radiat Environ Biophys. 2006;44:257-260.
8. International Commission on Radiological Protection. ICRP publication 26: recommendations of the ICRP. Ann ICRP. 1977;1.
9. International Committee on Radiological Protection. ICRP publication 103: the 2007 recommendations of the International Commission on Radiological Protection. Ann ICRP. 2007;37.
10. ICRP, Khong PL, Ringertz H, et al. ICRP publication 121: radiological protection in paediatric diagnostic and interventional radiology. Ann ICRP. 2013;42:1-63.
11. Rajaraman P, Doody MM, Yu CL, et al. Cancer risks in U.S. radiologic technologists working with fluoroscopically guided interventional procedures, 1994–2008. Am J Roentgenol. 2016;206:1101–1108.
12. Bartal One thousand, Roguin A, Paulo G. Telephone call for implementing a radiation protection civilisation in fluoroscopically guided interventional procedures. AJR Am J Roentgenol. 2016;206:1110–1111.
xiii. Walden C. Occupational exposure and adverse effects in the radiologic interventional setting. Radiol Technol. 2016;87:460-464.
14. European Commission. Radiation protection no 175: guidelines on radiation protection education and preparation of medical professionals in the Eu. Grand duchy of luxembourg: Publication Part of the European Marriage; 2014. Available at http://www.eurosafeimaging.org/wp/wp-content/uploads/2015/05/175.pdf. Accessed July 18, 2016.
xv. Vañó E, Rosenstein Thou, Liniecki J, et al. ICRP publication 113. Pedagogy and grooming in radiological protection for diagnostic and interventional procedures. Ann ICRP. 2009;39:seven-68.
16. Christodoulou EG, Goodsitt MM, Larson SC, et al. Evaluation of the transmitted exposure through lead equivalent aprons used in a radiology department, including the contribution from backscatter. Med Phys. 2003;30:1033-1038.
17. Oyar O, Kıslalıoglu A. How protective are the lead aprons we use against ionizing radiation? Diagn Interv Radiol. 2012;xviii:147-152.
Graciano Paulo, PhD
Section of Medical Imaging & Radiotherapy
IPC-ESTESC, Coimbra Health School
Coimbra, Portugal
graciano@estescoimbra.pt
Disclosures: None.
Gabriel Bartal, MD, FCIRSE, FSIR
Diagnostic and Interventional Radiology
Meir Medical Center
Sackler Medical School
Tel Aviv University
Tel Aviv, Israel
gbartal@gmail.com
Disclosures: None.
Eliseo Vañó, PhD
Radiology Department
Complutense University
Instituto de Investigación Sanitaria del Hospital
Clínico
San Carlos
Madrid, Spain
Disclosures: None.
Source: https://evtoday.com/articles/2016-aug/radiation-risk-to-radiographers-what-we-know
0 Response to "How Can People Protect Themselves From Exposure to Known Risks Factor's of Cancer?"
Post a Comment